SHRUTHI ARUKONDA 02
GENERAL MEDICINE.
28 July ,2021.
Note: This is an online E Log book recorded to discuss and comprehend our patient's de-identified health data shared, AFTER taking his/her/guardian's signed informed consent.
CASE REPORT
A 64 year old male with chief complaints of fever since 4 days, loose stools since 4 days , swelling of the left lower limb since a month and abdominal distension since one month .
CHEIF COMPLAINTS:
- Fever since 4 days. High grade a/w chills, decreases on medication.
- Loose stools since 4 days a/w mucoid, small volume, watery consistency
- Swelling of the left lower Limb since past one month
- Abdominal distension since past one month
- No h/o pain abdomen
- No h/o blood and pus in stools.
HISTORY OF PRESENT ILLNESS:
Nothing significant
HISTORY OF PAST ILLNESS:
K/c/o bronchial asthma
De novo detected DM ?
TREATMENT HISTORY:
Is on Asthma medication.
PERSONAL HISTORY:
Married.
Appetite - normal
Non vegetarian
Bowels- regular.
Micturition- abnormal
Known allergies - none
FAMILY HISTORY :
Nothing significant.
PHYSICAL EXAMINATION:
GENERAL :
No signs of pallor, icterus, clubbing of fingers or toes, lymphadenopathy or malnutrition.
Dehydration - yes
Oedema of feet - yes
VITALS:
- Temp- a febrile
- Pulse rate - 90/min
- Respiration rate-26/min
- Bp- 80[systolic]/60
- Spo2: 98% at 4L of o2
SYSTEMIC EXAMINATION:
CVS: S1S2 ++
RESPIRATORY SYSTEM:
- Dyspnoea - yes
- Position of trachea - central
- Breath sounds - vesicular
ABDOMEN :
- Shape of abdomen - scaphoid
- Tenderness - not
- Palpable mass- no
- Hernial orifices - normal
- Free fluid - no
- Bruits- no
- Liver- not palpable
- Spleen - not palpable.
- Bowel sounds - yes.
CNS:
Level of consciousness- conscious
Speech- normal
Signs of meningeal irritation- none
INVESTIGATIONS:
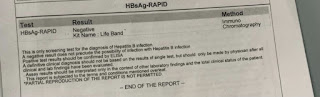
1.anti HCV antibodies - RAPID
PROVISIONAL DIAGNOSIS:
Acute gastroenteritis
With k/c/o bronchial Asthma
With de novo detected diabetes
With left lower limb cellulitis
?septic shock
TREATMENT:
DAY 1:
- IVF- NS and RL = 1000ml/hr
- Inj. Hydrocort 100mg iv
- CPAP ventilation
- Neb with budecort , 4th hourly
- Inj. HAI s/c acc to GRBS
- Tab sporlac DS po/TID
- Strict I/o monitoring
- Inj piptaz 4.5 gn IV/ stat
- Inj clindamycin 600mg IV/BD
DAY 2 :
- Inj streptokinase, 3 ml/hr
- Fluid restriction <1.5 l/ day
- Salt restriction <4gm/day
- Inj piptaz 2.25 gm /IV/ TID
- Inj clindamycin 600mg /IV/TID
- Inj. Hydrocortisone 100mg/IV/TID
- Inj. Neb with budecort 6th hourly
- Intermittent CPAP ventilation
- Strict I/o monitoring
- BP, PR, SPO2 monitoring hourly
- Inj. Heparin 1ml (1000IU) in 4 ml NS/IV/QID








Comments
Post a Comment